A 45-year-old man had type 2 diabetes mellitus of 2 years’ duration. He had no history of ischaemic heart disease or microvascular complications, and was euthyroid. There was no family history of ischaemic heart disease. He was a non-smoker and drank 4 to 8 units of alcohol per week. He was taking metformin only.
On examination, his blood pressure was 120/78 mmHg and his body mass index was 24 kg/m2 (18–25).
His calculated 10-year cardiovascular risk was 8.5%.
Investigations (fasting):
serum sodium142 mmol/L (137–144)
serum potassium3.8 mmol/L (3.5–4.9)
serum creatinine90 µmol/L (60–110)
haemoglobin A1c48 mmol/L (20–42)
urinary albumin:creatinine ratio1.5 mg/mmol (<2.5)
serum cholesterol5.1 mmol/L (<5.2)
serum HDL cholesterol1.50 mmol/L (>1.55)
fasting serum triglycerides1.22 mmol/L (0.45–1.69)
What does the NICE guidance (CG181, July 2014) on type 2 diabetes mellitus recommend as the most appropriate next step in management?
A 64-year-old man attended the diabetes clinic for annual review. He complained of very recent tingling in his feet. A monofilament was used to screen for the presence of chronic sensorimotor diabetic peripheral neuropathy.
What force should a monofilament deliver?
A 33-year-old woman, who was 9 weeks into her first pregnancy, was admitted with prolonged vomiting and secondary dehydration. She had lost 6 kg in weight since becoming pregnant. There was a strong family history of thyroid disease: two sisters were hypothyroid and one brother had required radioactive iodine for Graves’ disease.
On examination, she had a smooth, small goitre. Her pulse was 94 beats per minute and her blood pressure was 104/42 mmHg. There was a tremor of the outstretched hands. Urinalysis was normal.
Investigations:
serum sodium143 mmol/L (137–144)
serum potassium4.4 mmol/L (3.5–4.9)
serum creatinine105 µmol/L (60–110)
serum thyroid-stimulating hormone (TSH)<0.01 mU/L (0.4–5.0)
serum free T424.0 pmol/L (10.0–22.0)
serum free T311.0 pmol/L (3.0–7.0)
A TSH receptor antibody concentration was awaited.
In addition to rehydration, what is the most appropriate next step in the management of her abnormal thyroid function?
A 43-year-old man was in an ENT ward, having recently undergone removal of a carotid body tumour. Five years previously, he had undergone a similar procedure in another hospital. He also recalled that his brother had undergone surgery for a similar condition, and that his father, who had since died, might also have had neck surgery.
The ENT surgeons were concerned that there might be an underlying genetic diagnosis.
What is the most likely diagnosis?
A 17-year-old girl was referred to the transition clinic. She was taking hydrocortisone 10 mg twice daily and fludrocortisone 150 micrograms daily following a failed short tetracosactide (Synacthen®) test 5years previously. She had entered puberty at the age of 10 but had never achieved adult breast development or menarche.
Investigations:
haemoglobin95 g/L (115–165)
MCV124 fL (80–96)
white cell count8.4 ? 109/L (4.0–11.0)
platelet count334 ? 109/L (150–400)
serum sodium138 mmol/L (137–144)
serum potassium4.4 mmol/L (3.5–4.9)
serum urea3.5 mmol/L (2.5–7.0)
serum corrected calcium1.80 mmol/L (2.20–2.60)
serum follicle-stimulating hormone67.9 U/L (2.5–10.0)
serum luteinising hormone56.4 U/L (2.5–10.0)
What is the most likely diagnosis?
An 18-year-old man with cystic fibrosis was referred to clinic. Over recent months his lung function had deteriorated and he had lost weight. He was being treated for a chest infection at the time of the consultation.
Investigations:
oral glucose tolerance test (75 g):
fasting plasma glucose8.2 mmol/L (3.0–6.0)
2-h plasma glucose13.5 mmol/L (<7.8)
What is the most appropriate management?
A 47-year-old man presented with a 2-month history of polyuria and polydipsia. He awoke six times most nights to pass copious volumes of urine despite not drinking any fluid for 4 hours before going to bed.
Investigations:
MR scan of pituitary fossasee image
A water deprivation test confirmed the diagnosis of cranial diabetes insipidus.
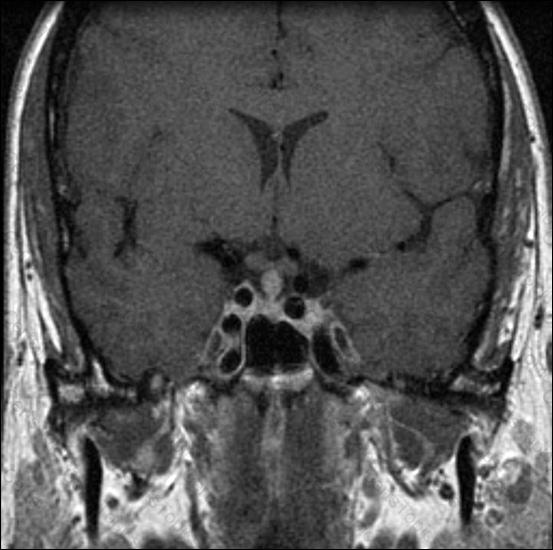
What is the most likely underlying diagnosis?
A 42-year-old woman presented with a 6-month history of tiredness. She also had a history of hypothyroidism, for which she was taking levothyroxine 150 micrograms daily, and a family history of hyperactivity syndrome.
Examination was normal.
Investigations:
serum thyroid-stimulating hormone12.3 mU/L (0.4–5.0)
serum free T418.0 pmol/L (10.0–22.0)
What is the most likely diagnosis?
A 26-year-old woman presented with recurrent Graves’ disease. After discussing the treatment options, she chose radioiodine.
What dose of radioiodine is most appropriate in uncomplicated Graves’ disease?
A 26-year-old woman with type 1 diabetes mellitus was seen in the antenatal diabetes clinic and was 8 weeks pregnant. The father of her child also had type 1 diabetes mellitus. They were concerned that their child might develop type 1 diabetes mellitus.
What is the likelihood of the child developing type 1 diabetes mellitus?
A 56-year-old man presented with a 6-month history of erectile dysfunction. He had noticed a gradual reduction in his frequency of shaving from daily to twice a week. His libido had diminished and he felt that he was not as strong as he once was. He also described general aches and pains. He was a farm worker and had drunk a bottle of vodka daily for several years, but had stopped drinking 2 years previously. He was a non-smoker.
Investigations:
serum urea6.2 mmol/L (2.5–7.0)
serum creatinine89 µmol/L (60–110)
serum albumin40 g/L (37–49)
serum total bilirubin17 µmol/L (1–22)
serum alanine aminotransferase48 U/L (5–35)
serum aspartate aminotransferase37 U/L (1–31)
haemoglobin A1c55 mmol/mol (20–42)
serum cortisol (09.00 h)389 nmol/L (200–700)
serum testosterone0.7 nmol/L (9.0–35.0)
plasma follicle-stimulating hormone2.1 U/L (1.0–7.0)
plasma luteinising hormone2.4 U/L (1.0–10.0)
serum prolactin458 mU/L (<360)
serum thyroid-stimulating hormone3.4 mU/L (0.4–5.0)
MR scan of pituitarysee image
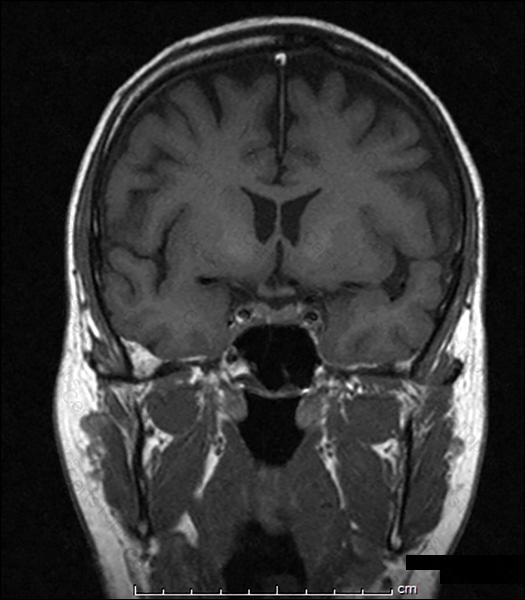
What is the most likely explanation of his symptoms?
A 73-year-old man had been attending the diabetes clinic for 6 weeks with an ulcer on his right second metatarsal head. He had been receiving regular podiatry and offloading.
What new feature in the appearance of his foot is most likely to suggest the need to start antibiotics?
A 55-year-old dental nurse was referred for bone densitometry after sustaining a non-displaced fracture of the femur after falling down a step. She had experienced no other fractures. Her only medical problem was long-standing anaemia of unknown cause. The only family history was of persistent dental abscesses affecting her father. She had three children who were well. She was taking no medication.
Examination was normal.
Investigations:
haemoglobin102 g/L (115–165)
MCV85 fL (80–96)
white cell count6.0 ? 109/L (4.0–11.0)
platelet count245 ? 109/L (150–400)
erythrocyte sedimentation rate25 mm/1st h (<30)
serum creatinine85 µmol/L (60–110)
serum corrected calcium2.40 mmol/L (2.20–2.60)
serum alkaline phosphatase56 U/L (45–105)
DXA scan spine (L2–L4)T score +5.8
DXA scan total hipT score +5.4
What is the most likely diagnosis?
A 76-year-old man with a 17-year history of type 2 diabetes mellitus attended for his annual review. Comparison of his retinal screening report with the previous year’s report showed that his visual acuity was unchanged at 6/9 in both eyes. The previous year’s right eye retinal image had been reported as ‘pre-proliferative retinopathy’, whereas this year’s was reported as ‘pre-proliferative retinopathy with maculopathy’.
What is the most appropriate next step?
A 32-year-old woman, with a 22-year history of type 1 diabetes mellitus, was seen in a pre-pregnancy diabetes clinic. She was a primigravida.
On examination, she had early background retinopathy, her blood pressure was 128/68 mmHg, and her body mass index was 29.7 kg/m2 (18–25).
Investigations:
haemoglobin A1c56 mmol/mol (20–42)
urinary albumin:creatinine ratio1.2 mg/mmol (<3.5)
Over the years her haemoglobin A1c concentration had varied between 58 and 69 mmol/mol. She had impaired awareness of hypoglycaemia and experienced approximately two severe hypoglycaemic events per year. She was worried about the risk of severe congenital malformations in her baby.
To what extent will the average risk of severe congenital malformation be increased in infants born to this mother with pregestational diabetes?
A 17-year-old Caucasian girl presented with primary amenorrhea.
On examination, her body mass index was 21 kg/m2 (18–25). Her body habitus was normal and she had appropriate breast development. There was no hirsutism or acne.
Investigations:
serum oestradiol<180 pmol/L (200–400)
serum testosterone31.7 nmol/L (0.5–3.0)
serum follicle-stimulating hormone4.0 U/L (2.5–10.0)
serum luteinising hormone6.0 U/L (2.5–10.0)
What is the most likely diagnosis?
A 34-year-old man was referred to the diabetes outpatient clinic with impaired glucose tolerance. He had a family history of diabetes mellitus and had a body mass index of 34.6 kg/m2 (18–25).
On examination, his blood pressure was 140/82 mmHg.
He wished to delay the onset of frank diabetes mellitus.
What is the most effective way of achieving this outcome?
A 55-year-old woman presented with thirst, polyuria and polydipsia. Her symptoms had started 9 months previously following a road traffic accident. Her past medical history was normal and she was not taking any regular medication.
On examination, her blood pressure was 130/80 mmHg with no postural drop. Urine volume measured 5 L in 24 hours.
Investigations:
serum sodium131 mmol/L (137–144)
serum potassium3.6 mmol/L (3.5–4.9)
serum urea2.0 mmol/L (2.5–7.0)
serum corrected calcium2.40 mmol/L (2.20–2.60)
fasting plasma glucose6.4 mmol/L (3.0–6.0)
serum osmolality278 mosmol/kg (278–300)
urinary osmolality100 mosmol/kg (100–1000)
What is the most likely diagnosis?
A 67-year-old woman presented to her general practitioner with a swelling in her neck. It had been present for 4–5 years and had not changed in size during that time. She was completely asymptomatic and remained well.
On examination, there was a nodular goitre and no lymphadenopathy.
Investigations:
serum thyroid-stimulating hormone1.1 mU/L (0.4–5.0)
A subsequent ultrasound scan demonstrated seven nodules bilaterally (ranging in size from 5 mm to 15 mm), which had no suspicious features.
What is the most appropriate next step in management according to British Thyroid Association 2014 Guidelines for the Management of Thyroid Cancer?
A 64-year-old woman presented with features of acromegaly. An MR scan showed a pituitary tumour with cavernous sinus extension. She underwent trans-sphenoidal surgery and histology of the pituitary tissue showed numerous cells immunostaining for growth hormone.
Investigations (6 months postoperatively):
MR scan of pituitaryenlarged sella, residual tumour in right cavernous sinus
serum growth hormone (day curve average)3.2 ?g/L (<2)
serum insulin-like growth factor 142.0 nmol/L (3.3–23.3)
What is the most appropriate next step in management?
A 33-year-old woman was reviewed in the insulin pump clinic. She had had type 1 diabetes mellitus for 10 years. She had been treated with a continuous subcutaneous insulin infusion 3 years previously, because of frequent hypoglycaemic episodes. She had recently undergone continuous glucose monitoring (see image).
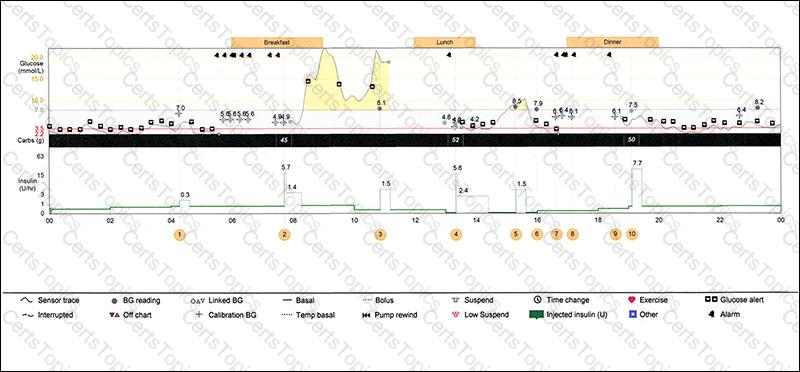
Investigations:
haemoglobin A1c43 mmol/mol (20–42)
What is the most likely cause of the blood glucose trace seen between 08.00 h and 10.00 h?
A 16-year-old boy was referred to the diabetes clinic following the discovery of a random plasma glucose concentration of 18.0 mmol/L. His general practitioner had begun treatment with metformin. The patient had a body mass index of 35 kg/m2 (18–25). He had had problems throughout his childhood, and had been taken out of school and was educated at home by his mother. He was attending the ophthalmology clinic for visual problems.
On examination, he was obese. He had hearing aids in both ears and evidence of acanthosis nigricans. Neither parent had a history of diabetes mellitus.
What is the most likely diagnosis?
A 24-year-old man was referred for investigation of infertility. He had been having unprotected intercourse with his partner for 18 months, but the couple had failed to conceive. He had been treated for Hodgkin’s lymphoma at the age of 17.
What is the most appropriate investigation?
A 66-year-old woman was admitted with carpopedal spasm. During the previous week she had had 2 days of diarrhoea following treatment with ciprofloxacin for a urinary tract infection. She had long-standing rheumatoid arthritis treated with prednisolone 5 mg daily, and was also taking alendronic acid, omeprazole and furosemide.
Investigations:
serum creatinine115 ?mol/L (60–110)
serum corrected calcium1.79 mmol/L (2.20–2.60)
serum alkaline phosphatase124 U/L (45–105)
serum magnesium0.26 mmol/L (0.75–1.05)
plasma parathyroid hormone2.7 pmol/L (0.9–5.4)
Which medicine is most likely to be responsible for her metabolic derangement?
A 67-year-old man underwent an isotope bone scan after being found to have a raised serum alkaline phosphatase (of bone origin). The blood test had been ordered because of mild lower back pain, which had now resolved. He was not taking any medication.
Examination was normal.
Investigations:
isotope bone scansee image
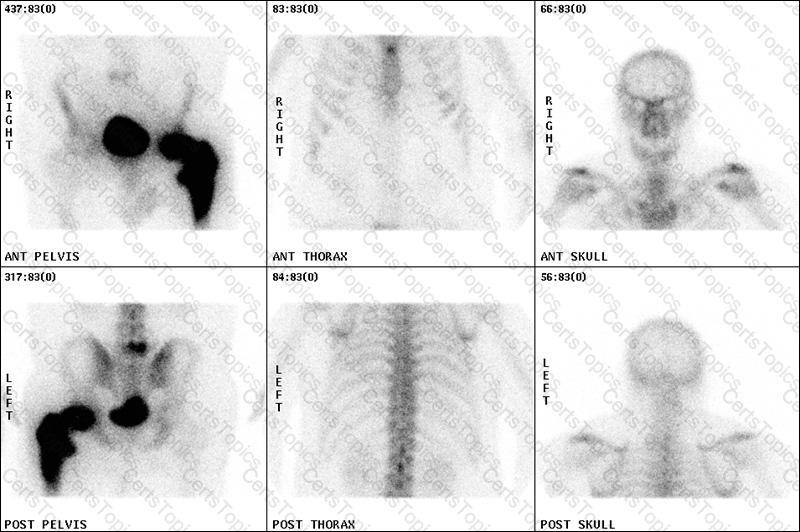
What is the most likely diagnosis?
A 73-year-old man with type 2 diabetes mellitus was reviewed because of deteriorating blood glucose control. He was taking metformin 850 mg twice daily.
On examination, his body mass index was 29 kg/m2 (18–25).
Investigations:
serum creatinine102 µmol/L (60–110)
haemoglobin A1c66 mmol/mol (20–42)
According to the NICE guidelines (CG87, May 2009), what would be the most appropriate additional treatment?
A 48-year-old woman presented with a 2-year history of weight gain, easy bruising and mood disturbance.
Investigations:
fasting plasma glucose6.9 mmol/L (3.0–6.0)
low-dose dexamethasone suppression test (2 mg/day for 48 h):
serum cortisol200 nmol/L (<50)
24-h urinary free cortisol (?3)670, 400 and 300 nmol (55–250)
plasma adrenocorticotropic hormone (09.00 h)25.0 pmol/L (3.3–15.4)
MR scan of pituitarynormal
What test is most likely to give a definitive diagnosis?
A 55-year-old woman presented with a 3-week history of nausea and vomiting. Her only medical complaints were frequent dyspepsia, for which she was taking indigestion tablets, and asthma for which she was taking a salbutamol inhaler as required.
On examination, there was no evidence of lymphadenopathy, her chest was clear on auscultation and abdominal examination was normal.
Investigations (before and after taking omeprazole for 3 weeks):
beforeafternormal
erythrocyte sedimentation rate (mm/1st h)44<30
serum creatinine (µmol/L)17011060–110
serum corrected calcium (mmol/L)2.852.402.20–2.60
serum phosphate (mmol/L)1.90.8–1.4
serum angiotensin-converting enzyme (U/L)8525–82
plasma parathyroid hormone (pmol/L)0.44.40.9–5.4
What is the most likely cause of the hypercalcaemia?
A 44-year-old man was referred for investigation of cortisol excess. He had poorly controlled hypertension, and a long history of type 2 diabetes mellitus with retinopathy and peripheral neuropathy. His medication comprised aspirin, ramipril, atenolol, carbamazepine, metformin and simvastatin.
Initial investigations:
serum cortisol (09.00 h)350 nmol/L (200–700)
serum cortisol (22.00 h)48 nmol/L (50–250)
overnight dexamethasone suppression test (after 1 mg dexamethasone):
serum cortisol93 nmol/L (<50)
24-h urinary free cortisol (day 1)225 nmol (55–250)
24-h urinary free cortisol (day 2)200 nmol (55–250)
24-h urinary free cortisol (day 3)185 nmol (55–250)
What is the most appropriate next step in management?
A pregnant 36-year-old woman presented to the diabetes outpatient clinic. She had type 2 diabetes mellitus treated with diet, lifestyle changes and metformin 500 mg twice daily.
On examination, her blood pressure was 128/84 mmHg.
Investigations:
haemoglobin A1c47 mmol/mol (20–42)
urinary albumin:creatinine ratio1.6 mg/mmol (<3.5)
Which is the best agent to reduce the risk of pre-eclampsia in this patient?