Satisfied with the outcome of a Requirements Workshop, a Business Analyst (BA) attributed the success to preparation. The assigned task had been to document the requirements for capturing details on vehicle incidents for Personal Auto.
Before the session, the BA reviewed ClaimCenter functionality by creating a new Personal Auto Claim involving physical damage to a vehicle.
During review, the BA saw that ClaimCenter did not have a graphical representation of a vehicle with clickable hot spots to identify the damage areas like they have in their current application.
Upon further research, the BA found that Guidewire does offer this functionality and even provides a Graphical Incident Capture Accelerator to ease implementation.
During the workshop, the BA was able to clearly present all options for capturing vehicle incident details. Instead of having to develop the Vehicle Incident Capture functionality from scratch, the team was able to make a quick decision to add this functionality and end the meeting 30 minutes early.
Which two outcomes demonstrate the importance of preparing for a Requirements Workshop by becoming familiar with the features and functionality of ClaimCenter? (Choose two.)
An Adjuster at Succeed Insurance creates a check with a partial payment of $1,200 for medical expenses payable to a claimant who was injured in a collision. The check has completed the following processing steps:
. The payment exceeded the Adjuster's authority limits, changing the status to Pending Approval.
. The Adjuster's supervisor reviewed and approved the payment, changing the status to Awaiting Submission.
. A batch process sent the check to the external check processing system, changing the status to Requested when ClaimCenter received an update from the external system.
The Adjuster received new information indicating that the check amount should be reduced to $950.
Which action should the Adjuster take?
Succeed Insurance needs the ability to associate a primary hospital with an injury incident if the injured party received treatment. When treatment is needed, the primary hospital name should display on the injury incident screen along with other details about the injury and treatment received.
The primary hospital should be added to the injury incident in one of the following ways:
. Select the name from a list of medical care organizations already associated with the claim.
. Enter the contact details directly in the incident.
. Search the Address Book from the incident to locate a hospital.
Which two requirements must be documented to associate the primary hospital with the claim? (Choose two.)
A claim for an auto accident in Tampa, Florida has been reported and recorded in ClaimCenter. The ClaimCenter base product Global Claim Assignment Rule is utilized for automatic assignment to Adjusters regardless of complexity of claims.
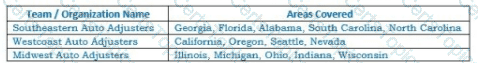
What is the likely path of assignment for this claim?