A patient presents with 26 skin tags on the neck and shoulder. The provider removes all using a scissoring technique.
What CPT® coding is reported?
A physician excises a 3.5 cm malignant lesion including margins from the back. Then a destruction of a 2.0 cm benign lesion on the right cheek of the face with cryosurgery.
What CPT@ and ICD-10-CM is reported?
A patient presents to the ER from a nursing home after the patient was found to have foul smelling, large sacral pressure ulcer during daily nursing rounds. The ER provider swabbed the wound
for culture (which measured at 7cm in largest diameter); then cleaned the site before painting with povidone around the entire sacrum to reduce cutaneous bacterial load. The provider made an
elliptical excision with 3mm margins around the outer edge of the ulcer and removed the lesion in its entirety. Further examination revealed deep tissue damage, prompting muscle and
segmental bone removal. The wound was then closed using a layered skin flap closure.
What CPT® coding and ICD-10-CM coding is reported?
Patient has cervical spondylosis with myelopathy. The surgeon performed a bilateral posterior laminectomy with facetectomies at each level and foraminotomies performed between interspaces C5-C6 and C6-C7. Bilateral decompression of the nerve roots is achieved.
What CPT® coding is reported?
What ICD-10-CM coding is reported for a patient who has hypertension and CKD stage 2?
What is the muscular ring around a lumen that contracts to control flow through that lumen called?
The patient came in with an inflamed seborrheic keratosis on her nose for a shave removal. After applying local anesthesia, a 0.7 cm dermal lesion was removed using an 11 blade.
What CPT® and ICD-10-CM codes are reported?
A 63-year-old is seen by his. primary care physician for an annual exam. His last exam with the primary care physician was four years ago. He has no complaints.
What CPT code is reported?
A patient who has colon adenocarcinoma undergoes an open partial colectomy. The surgeon removes the proximal colon and terminal ileum and reconnects the cut ends of the distal ileum and
remaining colon.
What procedure and diagnosis codes are reported?
The procedure is performed at an outpatient radiology department. From a left femoral access, the catheter is placed in the abdominal aorta and is then selectively placed in the celiac trunk and manipulated up into the common hepatic artery for an abdominal angiography. Dye is injected, and imaging is obtained. The provider performs the supervision and interpretation.
What CPT® codes are reported?
A surgeon performs a complete bilateral mastectomy with insertion of breast prosthesis at the same surgical session.
What CPT@ coding is reported?
Which entity offers compliance program guidance to form the basis of a voluntary compliance program for a provider practice?
Patient had polyps removed on a previous colonoscopy. The patient returns three months later for a follow-up examination for another colonoscopy. No new polyps are seen.
What diagnosis coding is reported for the second colonoscopy?
A 58-year-old with type 1 diabetes mellitus comes in for comprehensive eye examination. She is diagnosed with diabetic retinopathy with macular edema in the right eye. What ICD-10-CM coding is reported?
A 62-year-old with ventricular fibrillation comes to the outpatient surgery department for the replacement of a pacing cardioverter-defibrillator. The procedure is performed under MAC
anesthesia. The Certified Registered Nurse Anesthetist (CRNA), is working independently without medical direction.
What CPT® and ICD-10-CM codes are reported for the CRNA?
A patient is diagnosed with a healing pressure ulcer on her left heel that is currently being treated.
What ICD-10-CM coding is reported?
A patient undergoes a laparoscopic appendectomy for chronic appendicitis.
What CPT® and diagnosis codes are reported?
A catheter is placed from the femoral artery into the right common carotid, with imaging of the ipsilateral extracranial carotid and bilateral external carotids.
Which CPT® codes are reported?
A therapeutic colonoscopy is performed, where the scope goes beyond the splenic flexure, but not to the cecum. Using the Colonoscopy Decision Tree illustrated in the CPT® code book, what coding is reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® codes are reported?
Which is an anesthesia physical status modifier?
A 60-year-old male has three-vessel disease and supraventricular tachycardia which has been refractory to other management. He previously had pacemaker placement and stenting of LAD coronary artery stenosis, which has failed to solve the problem. He will undergo CABG with autologous saphenous vein and an extensive modified MAZE procedure to treat the tachycardia.
He is brought to the cardiac OR and placed in the supine position on the OR table. He is prepped and draped, and adequate endotracheal anesthesia is assured. A median sternotomy incision is made and cardiopulmonary bypass is initiated. The endoscope is used to harvest an adequate length of saphenous vein from his left leg. This is uneventful and bleeding is easily controlled. The vein graft is prepared and cut to the appropriate lengths for anastomosis. Two bypasses are performed: one to the circumflex and another to the obtuse marginal. The left internal mammary is then freed up and it is anastomosed to the ramus, the first diagonal, and the LAD. An extensive maze procedure is then performed and the patient is weaned from bypass. At this point, the sternum is closed with wires and the skin is reapproximated with staples. The patient tolerated the procedure without difficulty and was taken to the PACU.
Choose the procedure codes for this surgery.
Two weeks after removal of a 4 cm subcutaneous lipoma, the patient presents with extensive internal wound dehiscence requiring multi-layer closure in the OR.
What CPT® coding is reported by the surgeon?
View MR 003396
MR 003396
Operative Report
Preoperative Diagnosis: Acute MI, severe left main arteriosclerotic coronary artery disease
Postoperative Diagnosis: Acute MI, severe left main arteriosclerotic coronary artery disease
Procedure Performed: Placement of an intra-aortic balloon pump (IABP) right common femoral artery
Description of Procedure: Patient's right groin was prepped and draped in the usual sterile fashion. Right common femoral artery is found, and an incision is made over the artery exposing it. The artery is opened transversely, and the tip of the balloon catheter was placed in the right common femoral artery. The balloon pump had good waveform. The balloon pump catheter is secured to his skin after local anesthesia of 2 cc of 1% Xylocaine is used to numb the area. The balloon pump is secured with a 0-silk suture. The patient has sterile dressing placed. The patient tolerated the procedure. There were no complications.
What CPT® coding is reported for this case?
A patient underwent a colonoscopy, where the gastroenterologist biopsied two polyps from the colon. Each polyp was sent to pathology as separately identified specimens. The gastroenterologist was requesting a pathology consult while the patient was still on the table. Tissue blocks and frozen sections were then prepared and examined as follows:
Specimen 1: First Tissue Block—Three Frozen Sections Second Tissue Block—One Frozen Section Specimen 2: First Tissue Block—Two Frozen Sections Second Tissue Block—One Frozen Section
What CPT® coding is reported?
A business requires drug testing for cocaine and methamphetamines prior to hiring a job candidate. A single analysis with direct optical observation is performed, followed by a confirmation for cocaine.
Which codes are used for reporting the testing and confirmation?
An air bag deployed when a driver lost control of the car and crashed into a guardrail on the side of the highway. The driver suffers partial impact resulting in a skull fracture of the anterior
cranial base. The fracture is diagnosed using the MRI scanner and cerebrospinal fluid is noted dripping via the sphenoid sinus into the right nasal passage. The patient requires a surgical nasal
sinus endoscopy to assess and repair the injury.
What is the correct procedure and diagnosis coding combination to report this service?
A wedge excision of soft tissue at the lateral margin of an ingrown toenail on the left great toe is performed.
What CPT® code is reported?
The patient has a ruptured aneurysm in the popliteal artery. The provider makes an incision below the knee and dissects down and around the popliteal artery. After clamping the distal and
proximal ends of the artery, the provider cuts out the defect, sutures the remaining ends of the artery together, and places a patch graft to fill the gap. What is the correct CPT® code for the
aneurysm repair?
An interventional radiologist performs an abdominal paracentesis using fluoroscopic guidance to remove excess fluid. The procedure is performed in the hospital. What CPT® coding is reported?
Which statement regarding lesion excision is TRUE?
View MR 099405
MR 099405
CC: Shortness of breath
HPI: 16-year-old female comes into the ED for shortness of breath for the last two days. She is an asthmatic.
Current medications being used to treat symptoms is Advair, which is not working and breathing is getting worse. Does not feel that Advair has been helping. Patient tried Albuterol for persistent coughing, is not helping. Coughing 10-15 minutes at a time. Patient has used the Albuterol 3x in the last 16 hrs. ED physician admits her to observation status.
ROS: No fever, no headache. No purulent discharge from the eyes. No earache. No nasal discharge or sore throat. No swollen glands in the neck. No palpitations. Dyspnea and cough. Some chest pain. No nausea or vomiting. No abdominal pain, diarrhea, or constipation.
PMH: Asthma
SH: Lives with both parents.
FH: Family hx of asthma, paternal side
ALLERGIES: PCN-200 CAPS. Allergies have been reviewed with child’s family and no changes reported.
PE: General appearance: normal, alert. Talks in sentences. Pink lips and cheeks. Oriented. Well developed. Well nourished. Well hydrated.
Eyes: normal. External eye: no hyperemia of the conjunctiva. No discharge from the conjunctiva
Ears: general/bilateral. TM: normal. Nose: rhinorrhea. Pharynx/Oropharynx: normal. Neck: normal.
Lymph nodes: normal.
Lungs: before Albuterol neb, mode air entry b/l. No rales, rhonchi or wheezes. After Albuterol neb. improvement of air entry b/l. Respiratory movements were normal. No intercostals inspiratory retraction was observed.
Cardiovascular system: normal. Heart rate and rhythm normal. Heart sounds normal. No murmurs were heard.
GI: abdomen normal with no tenderness or masses. Normal bowel sounds. No hepatosplenomegaly
Skin: normal warm and dry. Pink well perfused
Musculoskeletal system patient indicates lower to mid back pain when she lies down on her back and when she rolls over. No CVA tenderness.
Assessment: Asthma, acute exacerbation
Plan: Will keep her in observation overnight. Will administer oral steroids and breathing treatment. CXR ordered and to be taken in the morning.
What E/M code is reported?
A mother brings her 2-year-old son to the pediatrician's office because he stuck a bead up his left nostril. The pediatrician uses a nasal decongestant to open the blocked nostril and removes the bead with nasal forceps.
What CPT® coding is reported?
A patient arrives for a PEG placement. The patient requires tube feeds for nutrition but frequently pulls out the dobhoffs tube. An EGD was performed. Several attempts were made to place the
PEG tube without success so the procedure was aborted. During the withdraw of the scope, a small hiatal hernia was noted in the stomach. The scope was removed the the patient transferred
to recovery.
What CPT and ICD-10-CM coding is reported?
A patient is seen at the doctor's office for nausea, vomiting, and sharp right lower abdominal pain. CT scan of the abdomen is ordered. Labs come back indicating an increased WBC count with review of the abdominal CT scan. The physician determines the patient has a ruptured appendicitis. The physician schedules an appendectomy and takes the patient to the operating room. The appendix is severed from the intestines and removed via scope inserted through an umbilical incision. What CPT® and diagnosis codes are reported?
A 65-year-old gentleman presents for refill of medications and follow-up for his chronic conditions. The patient indicates good medicine compliance. No new symptoms or complaints.
Appropriate history and exam are obtained. Labs that were ordered from previous visit were reviewed and discussed with patient. The following are the diagnoses and treatment:
Hypokalemia - stable. Refill Potassium 20 MEQ
Hypertension - blood pressure remaining stable. Patient states home readings have been in line with goals. Refill prescription Lisinopril.
Esophageal Reflux - Patient denies any new symptoms. Stable condition. Continue taking over the counter Prevacid oral capsules, 1 every day.
Patient is instructed to follow up in 3 months. Labs will be obtained prior to visit.
What CPT® code is reported?
The surgeon performs Roux-en-Y anastomosis of the extrahepatic biliary duct to the gastrointestinal tract on a 45-year-old patient.
What CPT® code is reported?
Which government office is responsible for overseeing and investigating cases of healthcare fraud and abuse?
An abdominal X-ray includes decubitus, supine, and erect views.
What CPT® code is reported?
Day 1 - A provider admits the patient to observation care for type 2 diabetes mellitus with hyperglycemia. The provider orders a HbA1c, a urine (microalbumin), and kidney function lab tests.
Blood sugar is high and poorly controlled. The provider discusses the case with the patient's endocrinologist. The provider prescribes an IV insulin drip, along with SQ insulin and keeps the
patient in observation overnight.
Day 2 - Patient is in observation care and the provider orders a blood glucose test. The patient's glucose levels have improved. The provider places an order for the dietitian to see the patient.
Provider
documents spending a total time of 25 minutes with the patient.
Day 3 - Patient has a blood glucose test. The patient's glucose level is back to normal. The provider documents spending 15 minutes with the patient. The provider discharges the patient.
What E/M coding is reported by the physician for the patient in observation care?
An established patient presents with fever and sore throat. Rapid strep test is positive.
What CPT® and ICD-10-CM codes are reported?
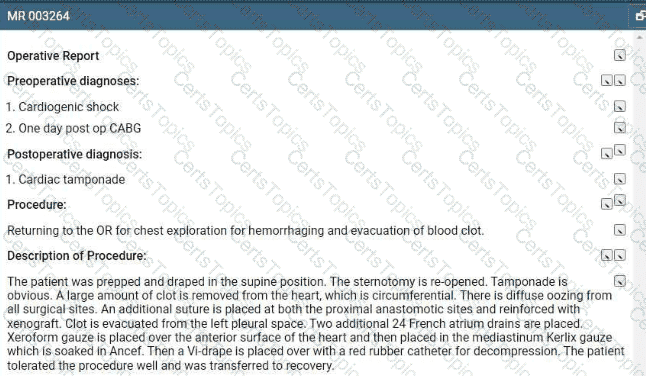
Refer to the supplemental information when answering this question:
View MR 003264
What is the procedural coding?
A patient has nausea with several episodes of emesis along with severe stomach pain due to dehydration. Normal saline is infused in the same bag with 2 mg ondansetron to help with the
nausea. Then a dose of 15 mg ketorolac tromethamine was given for the stomach pain.
What J codes are reported for these services?
A male patient passes out while jogging in the park. Upon examination at the hospital, he is found to have a wide complex tachycardia and undergoes an electrophysiologic study and radiofrequency ablation. For this procedure he is placed under general anesthesia.
What is the anesthesia coding for this otherwise healthy 35-year-old?
A 23-year-old receives MMR and Hepatitis B vaccines without counseling.
What CPT® codes are reported?
A patient presents for a percutaneous needle biopsy of the liver with ultrasound guidance to assess the severity of his primary biliary cirrhosis.
What CPT® and ICD-10-CM codes are reported?
View MR 007400
MR 007400
Radiology Report
Patient: J. Lowe Date of Service: 06/10/XX
Age: 45
MR#: 4589799
Account #: 3216770
Location: ABC Imaging Center
Study: Mammogram bilateral screening, all views, producing direct digital image
Reason: Screen
Bilateral digital mammography with computer-aided detection (CAD)
No previous mammograms are available for comparison.
Clinical history: The patient has a positive family history (mother and sister) of breast cancer.
Mammogram was read with the assistance of GE iCAD (computerized diagnostic) system.
Findings: No dominant speculated mass or suspicious area of clustered pleomorphic microcalcifications is apparent Skin and nipples are seen to be normal. The axilla are unremarkable.
What CPT® coding is reported for this case?
A patient was in a car accident as the driver and suffered a concussion with brief loss of consciousness (15 minutes). What ICD-10-CM codes are reported?
A patient is taken to the radiology department for a radiological cardiac catheterization. An acute MI of the left anterior descending coronary artery is found. The cardiologist performs a suction thrombectomy, followed by atherectomy and a stent to the artery. A CRNA provides MAC for this patient, who is status P5.
What code/modifier combination would you report for the services of the CRNA?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What E/M coding is reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® and ICD-10-CM codes are reported?
A patient presents to the emergency room with a nosebleed that is controlled by limited anterior nasal packing.
What CPT® code is reported?
A patient arrives with stridor and in respiratory distress. The provider performs a micro laryngoscopy using a Parson's laryngoscope and magnifying telescope. A bronchoscopy was also
performed using a 2.5 Stortz bronchoscope. The findings include subglottic web and stenosis with laryngeal edema suggestive of reflux. There was also significant collapse of the trachea at
the carina and into the main bronchi bilaterally.
What CPT® coding is reported?
A 42-year-old male is diagnosed with a left renal mass. Patient is placed under general anesthesia and in prone position. A periumbilical incision is made and a trocar inserted. A laparoscope is inserted and advanced to the operative site. The left kidney is removed, along with part of the left ureter. What CPT® code is reported for this procedure?
A patient suffers a ruptured infrarenal abdominal aortic aneurysm requiring emergent endovascular repair. An aorto-aortic tube endograft is positioned in the aorta and a balloon dilation is performed at the proximal and distal seal zones of the endograft. The balloon angioplasty is performed for endoleak treatment.
What CPT® code does the vascular surgeon use to report the procedure?
A patient with compression fractures of L5 and the sacrum undergoes vertebroplasty, with cement injected into two vertebral bodies, performed bilaterally.
What CPT® coding is reported?
According to the Application of Cast and Strapping CPT® guidelines, what is reported when an orthopedic provider performs initial fracture care treatment for a closed scaphoid fracture of the wrist, applies a short arm cast, and the patient will be returning for subsequent fracture care?
A patient who is 37 weeks' gestation is admitted to labor and delivery for a cesarean delivery. An external cephalic version was performed successfully several days ago and she now presents in labor, fully dilated, and the fetus has returned to a footling presentation.
What anesthesia code is reported?
A patient with multiple atypical lesions on the face and trunk is in the office to perform a biopsy. A punch tool was used to obtain a full-thickness tissue sample for two lesions on the trunk.
Partial-thickness tissue sample was taken from one lesion on the forehead using a curette.
What CPT® coding is reported?
A 4-year-old, critically ill child is admitted to the PICU from the ED with respiratory failure due to an exacerbation of asthma not manageable in the ER. The PICU provider takes over the care of the patient and starts continuous bronchodilator therapy and pharmacologic support with cardiovascular monitoring and possible mechanical ventilation support.
What is the E/M code for this encounter?
A pediatrician removes impacted cerumen using irrigation in the right ear and instrumentation in the left ear.
What CPT® coding is reported?
A patient undergoes an MRI of the lumbar spine without and with contrast for left-sided low back pain with sciatica.
What CPT® and ICD-10-CM codes are reported?
View MR 099401
MR 099401
Established Patient Office Visit
Chief Complaint: Patient presents with bilateral thyroid nodules.
History of present illness: A 54-year-old patient is here for evaluation of bilateral thyroid nodules. Thyroid ultrasound was done last week which showed multiple thyroid masses likely due to multinodular goiter. Patient stated that she can “feel" the nodules on the left side of her thyroid. Patient denies difficulty swallowing and she denies unexplained weight loss or gain. Patient does have a family history of thyroid cancer in her maternal grandmother. She gives no other problems at this time other than a palpable right-sided thyroid mass.
Review of Systems:
Constitutional: Negative for chills, fever, and unexpected weight change.
HENT: Negative for hearing loss, trouble swallowing and voice change.
Gastrointestinal: Negative for abdominal distention, abdominal pain, anal bleeding, blood in stool, constipation, diarrhea, nausea, rectal pain, and vomiting
Endocrine: Negative for cold Intolerance and heat intolerance.
Physical Exam:
Vitals: BP: 140/72, Pulse: 96, Resp: 16, Temp: 97.6 °F (36.4 °C), Temporal SpO2: 97%
Weight: 89.8 kg (198 lbs ), Height: 165.1 cm (65”)
General Appearance: Alert, cooperative, in no acute distress
Head: Normocephalic, without obvious abnormality, atraumatic
Throat: No oral lesions, no thrush, oral mucosa moist
Neck: No adenopathy, supple, trachea midline, thyromegaly is present, no carotid bruit, no JVD
Lungs: Clear to auscultation, respirations regular, even, and unlabored
Heart: Regular rhythm and normal rate, normal S1 and S2, no murmur, no gallop, no rub, no click
Lymph nodes: No palpable adenopathy
ASSESSMENT/PLAN:
1) Multinodular goiter - the patient will have a percutaneous biopsy performed (minor procedure).
What E/M code is reported for this encounter?
A patient is sent to the hospital by his family care provider for admission due to a high fever and neck pain The patient is admitted to the hospital to rule out bacterial meningitis. The hospitalist admits the patient and orders a CBC. CMR Blood culture, CT of the head and chest, and a lumbar puncture (spinal tap). After review of the results, he determines the patient has bacterial meningitis and starts the patient on IV antibiotics.
What CPT® and ICD-10-CM codes are reported for the admission?
A 58-year-old male suffered an acute STEMI of the inferolateral wall while running a marathon on June 15 and had received treatment. Three weeks later, the patient presents to the ED complaining of SOB and left arm pain. An EKG is performed as well as blood tests. Patient is admitted for further evaluation.
What diagnosis code is reported for this encounter?
A healthy 35-year-old undergoes EP study and ablation under general anesthesia.
What anesthesia coding is correct?
A patient with intermittent asthma with exacerbation undergoes spirometry before and after bronchodilator.
What CPT® and ICD-10-CM codes are reported?
In medical terminology, suffixes indicate the procedure, condition, disorder, or disease.
Which term contains a suffix?
Which is a TRUE statement for Place of Service (POS) codes for professional claims?
A patient presents with keratosis lesions on her left cheek, above the left eyebrow, and on the chin area. The dermatologist treats those areas by lightly sanding the surface of a total of 5 lesions.
What CPT® coding is reported?
A 32-year-old is in the outpatient clinic for an esophagoscopy due to increased difficulty swallowing with his eosinophilic esophagitis. The flexible scope is inserted in the mouth and into the
esophagus. Examination of the esophagus noted narrowing in the distal esophagus. Following an injection of Kenalog, a transendoscopic balloon dilation was performed in the area of
stenosis. Inflation was repeated eventually reaching 18 mm in diameter. What CPT® coding is reported for this procedure?
A temporary steroid-releasing sinus implant is placed in the ethmoid sinus.
What HCPCS Level II code is reported?
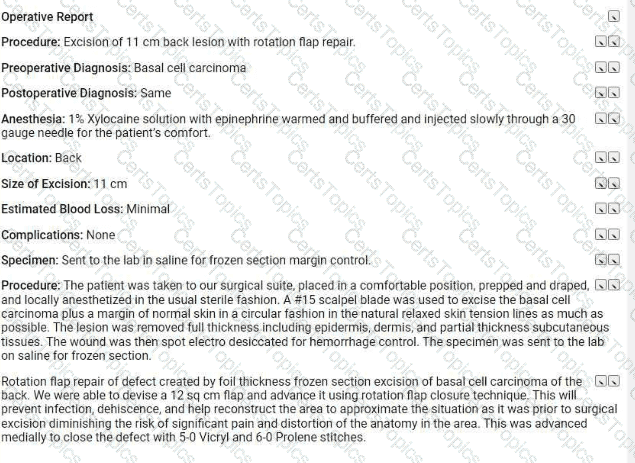
Refer to the supplemental information when answering this question:
View MR 623654
What CPTO coding is reported for this case?
Patient is admitted in observation care on 12/2/20XX in the morning for acute asthma exacerbation. The ED physician requires the patient to stay overnight. Next day, 12/3/20XX the patient is
discharged from observation care in the afternoon. Patient's total stay in observation was 16 hours.
What E/M categories and code ranges are appropriate to report?
A patient presents for planned sterilization via bilateral excisional vasectomy.
What CPT® and ICD-10-CM codes are reported?
A 30-year-old patient with a scalp defect is having plastic surgery to insert tissue expanders. The provider inserts the implants, closes the skin, and increases the volume of the expanders by injecting saline solution. Tissue is expanded until a satisfactory aesthetic outcome is obtained to repair the scalp defect.
What CPT® code is reported?
When a provider’s documentation refers to use, abuse, and dependence of the same substance (e.g., alcohol), which statement is correct?
A 44-year-old female patient came in for a planned laparoscopic total abdominal hysterectomy for endometriosis of the uterus. The surgeon attached the trocars, a scope is inserted examining
the uterus, abdominal wall, bilateral ovaries, and fallopian tubes. The surgeon decided to convert the laparoscopic procedure to an open total hysterectomy because of the extensive amount of
adhesions that need to be removed. A total hysterectomy was performed and due to removal of the extensive adhesions the surgery took longer than normal of 2 hours.
What CPT® and diagnosis codes are reported?
What is the medical term for a procedure that creates a connection between the gallbladder and the small intestine?
A patient undergoes right thyroid lobectomy for malignancy and removal of a suspicious parathyroid gland.
What CPT® codes are reported?
A patient returns for embryo transfer. The lab thaws cryopreserved embryos and cultures them for two additional days.
What CPT® coding is reported?
Provider performs staged procedures for gender reassignment surgery converting female anatomy to male anatomy.
What CPT® code is reported?
A patient with end-stage renal disease (ESRD) receives hemodialysis 3x weekly in the office for one month. The nephrologist performs a comprehensive exam and supervises dialysis.
What CPT® and ICD-10-CM codes are reported?
A patient presents to the urgent care facility with multiple burns acquired while burning debris in his backyard. After examination the physician determines the patient has third-degree burns of the left and right posterior thighs (10%). He also has second-degree burns of the anterior portion of the right side of his chest wall (8%) and upper back (6%). TBSA is 24% with third-degree burns totaling 10%.
What ICD-10-CM codes are reported, according to 1CD-10-CM coding guidelines?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What is the radiology coding for this encounter?
A patient has a bone infection being treated with vancomycin. A therapeutic drug assay is performed to measure the concentration of vancomycin in the patient's blood.
What lab test is reported?
A patient had surgery a year ago to repair two extensor tendons in his wrist. He is in surgery for a secondary repair for the same two tendons with free graft. What CPT® coding is reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® coding is reported?
A 10-year-old had a cochlear implant in his left ear few weeks ago. Today he sees the audiologist to initialize and program the implant.
What CPT® code is reported?
A physician sees a patient for the first observation visit, spends 85 minutes, with moderate MDM.
What CPT® code is reported?
Four malignant peritoneal tumors are excised, the largest measuring 15 cm.
What CPT® and ICD-10-CM coding is reported?
Which circumstance supports medical necessity for a payment by the insurance company?
A 60-year-old male suffering from degenerative disc disease at the L3-L4 and L5-S1 levels was placed under general anesthesia. Using an anterior approach, the L3-L4 disc space was exposed. Using blunt dissection, the disc space was cleaned. The disc space was then sized and trialed. Excellent placement and insertion of the artificial disc at L3-L4 was noted. The area was inspected and there was no compression of any nerve roots. Same procedure was performed on L5-S1 level. Peritoneum was then allowed to return to normal anatomic position and entire area was copiously irrigated. The wound was closed in a layered fashion. The patient tolerated the discectomy and arthroplasty well and was returned to recovery in good condition. What CPT® coding is reported for this procedure?
The patient, who is at 32 weeks pregnant, has been hospitalized due to an infection of COVID-19.
What ICD-10-CM codes are reported?
A witness of a traffic accident called 911. An ambulance with emergency basic life support arrived at the scene of the accident. The injured party was stabilized and taken to the hospital. What HCPCS Level II coding is reported for the ambulance's service?
A patient comes to the gynecologist's office to check if she is pregnant. A urine sample is taken and tested. The visual result is positive that she is pregnant.
What CPT® code is reported'
A patient with abnormal growth had a suppression study that included five glucose tests and five human growth hormone tests.
What CPT@ coding is reported?
A 49-year-old patient arrives with hearing loss in his left ear. Impedance testing via tympanometry is performed.
What CPT® code is reported?
Ten-year-old boy has a painful felon abscess of the deep tissues of the palmar surface of his right thumb. The provider makes an incision on one side of the nail and then across the fingertip parallel to the end of the nail. He identifies the area of abscess and drains it. A drainage tube is inserted.
What CPT® and ICD-10-CM is reported?
The human shoulder is made of which three bones?
Which CPT® code can append modifier 50?
A pediatrician is requested to attend a high-risk delivery and performs initial stabilization of the newborn after cesarean delivery.
What E/M service is reported?
The documentation states:
He was then sterilely prepped and draped along the flank and abdomen in the usual sterile fashion. I first made a skin incision off the tip of the twelfth rib, extending medially along the banger’s lines of the skin. This was approximately 3.5 cm in length. Once this incision was carried sharply, electrocautery was used to gain access through the external oblique, internal oblique, and transverse abdominis musculature and fascia.
What surgical approach was used for this procedure?
The provider orders a bile test for a patient that has chronic hepatitis that is undergoing treatment. Lab analyst quantitates the total bile acids with an enzymatic method. What CPT® code is
reported for the test?
A patient comes in complaining of pain in the lower left back, which is accompanied by a numbing sensation that extends into the leg. Attempts to alleviate the pain with home treatments have been unsuccessful. The provider orders an MRI of the lumbar spine initially without, and then with, contrast material. The images are interpreted by the physician, the final diagnosis is left-sided low back pain with sciatica.
What CPT® and ICD-10-CM codes are reported?
A 45-year-old patient presents with right shoulder pain. The provider administers three trigger point injections in the trapezius muscle and two in the pectoralis muscle.
What CPT® coding is reported?